Andrew Bowman, a veterinary epidemiologist at Ohio State College, had a hunch. He had been struck by the large quantities of H5N1 virus he’d seen in milk from cows contaminated with the hen flu and thought that a minimum of some virus was getting off of farms and going downstream — onto retailer cabinets.
He knew the Meals and Drug Administration was working by itself nationwide survey of the milk provide. However he was impatient. So he and a graduate scholar went on a highway journey: They collected 150 business milk merchandise from across the Midwest, representing dairy processing crops in 10 totally different states, together with some the place herds have examined constructive for H5N1. Genetic testing discovered viral RNA in 58 samples, he informed STAT.
The researchers anticipate further lab research at the moment underway to indicate that these samples don’t comprise reside virus with the potential to trigger human infections, which means that the danger of pasteurized milk to shopper well being continues to be very low. However the prevalence of viral genetic materials within the merchandise they sampled recommend that the H5N1 outbreak is probably going way more widespread in dairy cows than official counts point out. Thus far, the U.S. Division of Agriculture has reported 33 herds in eight states have examined constructive for H5N1.
“The truth that you possibly can go right into a grocery store and 30% to 40% of these samples check constructive, that means there’s extra of the virus round than is at the moment being acknowledged,” stated Richard Webby, an influenza virologist who has been analyzing the samples at St. Jude’s Youngsters’s Analysis Hospital in Memphis, Tenn., the place he heads the WHO Collaborating Middle for Research on the Ecology of Influenza in Animals.
Earlier this week, the FDA introduced that its effort had discovered proof of the H5N1 virus in samples of milk bought from retailer cabinets, however it offered no detailed outcomes. On Thursday, throughout an internet symposium hosted by the Affiliation of State and Territorial Well being Officers, the FDA disclosed a high-level readout from the company’s investigation. Outcomes returned Thursday morning confirmed PCR-positive milk in 20% of samples, “perhaps with some preponderance for areas with recognized herds,” stated Donald Prater, performing director of the FDA’s Middle for Meals Security and Utilized Vitamin. He didn’t say what number of samples the FDA had analyzed or from what geographic space.
The testing by PCR — polymerase chain response — turned up solely genetic traces of the virus, not proof that it’s alive or infectious. The FDA has been adamant that H5N1, which is heat-sensitive, may be very probably killed by way of the method of pasteurization.
The company continues to be assessing these samples for viral viability by trying to develop virus from milk discovered to comprise RNA from H5N1. The FDA plans to launch outcomes of these research within the coming days. On Wednesday, Jeanne Marrazzo, the brand new director of the Nationwide Institute of Allergy and Infectious Ailments, informed reporters {that a} crew of NIAID-funded researchers had early information to recommend that pasteurization does look like efficient.
The crew that produced that information — the St. Jude and OSU teams — informed STAT that it has thus far analyzed 4 samples of store-bought milk that had examined constructive through PCR for H5N1 genetic materials. “We’ve achieved the viral development assays to see if we will get well any virus from them and we will’t,” Webby stated.
These 4 samples got here from an preliminary assortment of twenty-two business milk merchandise bought within the Columbus, Ohio, space. “It was principally simply me hitting up the 5 grocery shops between campus and my home,” stated Bowman.
PCR testing at OSU revealed three of these 22 merchandise to be constructive for viral RNA. Bowman despatched them to Webby to inject into plates of mammalian cells and embryonated hen eggs and search for any indicators of lively viral replication. With the intention to do this, Webby wanted a adverse management, so he went and acquired milk at a retailer close to his lab in Memphis. However PCR testing discovered H5N1 RNA in that pattern too, making it ineffective as a adverse management, however an extra information level exhibiting an absence of reside virus.
That pattern continues to be in Webby’s fridge at dwelling. He used it to make dinner earlier this week. “I’m not involved about all of it,” he stated.
Though the danger of an infection from dairy merchandise may be very low, the fear is that the broader H5N1 spreads in cows, the extra alternatives the virus has to adapt to transmit effectively in mammalian hosts. It additionally enhance the possibilities H5N1 may get into pigs, the place it may swap genes and type hybrids with different flu viruses. Viruses that mutate to have the ability to unfold simply by way of one species of mammals may discover it simpler to contaminate folks.
The St. Jude group is now repeating its analyses with the extra samples Bowman and his graduate scholar purchased across the Midwest. Their early findings present additional proof that H5N1 is spreading broadly amongst dairy cows within the U.S.
This week, researchers analyzing viral genome sequences launched Sunday by the USDA discovered that the outbreak has probably been underway for months longer than beforehand recognized. “Each of those information — the milk information and the genetic information that exhibits this has been round since December of final 12 months — means that the outbreak might be a lot larger than we all know,” stated Angie Rasmussen, a virologist who research rising zoonotic pathogens on the Vaccine and Infectious Illness Group on the College of Saskatchewan in Canada.
It could additionally sign that herds will be infectious with solely delicate signs or no signs in any respect, which might complicate the response and make containment way more tough.
“That is telling us that we’re in all probability already seeing that milk from asymptomatically contaminated cows does have some virus in there,” stated Andrew Pekosz, a molecular microbiologist who research respiratory viruses at Johns Hopkins Bloomberg Faculty of Public Well being.
Thus far, there was solely one report of H5N1 infections in a cattle herd with no signs — in North Carolina. However USDA officers haven’t disclosed additional particulars past the truth that milk from contaminated however asymptomatic cows appears unchanged.
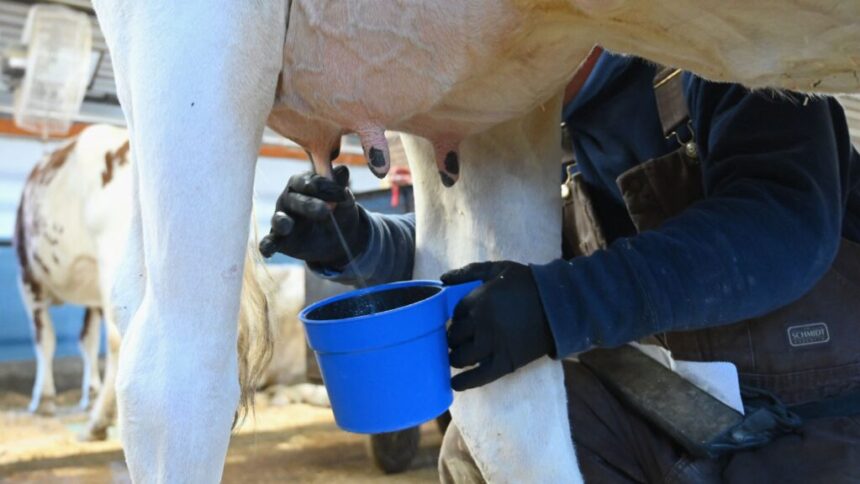
In H5N1-infected cows, the very first thing that tends to occur is their urge for food disappears and their exercise goes down. Then their milk manufacturing dries up. In some animals, the milk they do produce turns yellow and thick. “It’s an odd factor that appears to be distinctive to this explicit virus,” stated Keith Poulsen, director of the Wisconsin Veterinary Diagnostic Laboratory. And it’s one of many chief purple flags that dairy farmers are speculated to be looking out for when deciding whether or not to check their herds. If milk from asymptomatic or pre-symptomatic cows seems to be regular however can carry virus, it could obscure the necessity for testing.
To essentially perceive the size of unfold in addition to potential mechanisms of viral transmission, it’s essential to conduct widespread testing of animals with and with out signs, stated Jennifer Nuzzo, an epidemiologist and director of Brown College’s Pandemic Middle. “If we’re solely testing cows with outward signs, we’re lacking infections in these with out.”
Up till this week, USDA coverage didn’t require testing of any animals, and solely advisable it for dairy cows higher than 3 years of age which were lactating for a minimum of 150 days and are exhibiting extreme scientific signs like fever, lethargy, irregular milk manufacturing, and free stool.
On Wednesday, the company issued a federal order requiring an animal to check adverse for the virus earlier than it may be transported throughout state strains. It additionally requires laboratories and state veterinarians to report back to the USDA any animals which have examined constructive for H5N1 or some other influenza A virus. However outdoors of interstate journey, testing stays voluntary and inspired just for visibly ailing animals.
Public well being specialists informed STAT that such slim testing standards are probably distorting the true extent of the outbreak. “I’ve not seen proof that makes me wish to discard the worry that testing practices are completely shaping what we expect we learn about this virus,” Nuzzo stated. “We simply don’t have the appropriate information proper now to inform us what’s occurring.”
The scenario is reminiscent, she stated, of the Covid-19 pandemic. Within the early weeks of that outbreak, testing insurance policies have been slim — restricted to symptomatic people who had traveled to China. In the meantime, the SARS-CoV-2 virus was spreading undetected all through the U.S., as genomic analyses would later present. Later, when at-home checks grew to become extensively accessible, official counts grew to become unreliable, leaving state and native well being departments at nighttime.
“At the least with Covid, wastewater surveillance finally kicked in to complement our image,” Nuzzo stated. “With H5N1, we don’t have that.”
On Wednesday, the Facilities for Illness Management and Prevention stated it’s exploring wastewater testing for H5N1, however famous important hurdles, together with farms not being linked to municipal wastewater methods and the potential for contaminated wild birds to confound testing of water round farms.
Requiring dairy farms to frequently check all their animals, together with asymptomatic ones, shouldn’t be logistically possible given the present capability of state veterinary diagnostic laboratories, Poulsen stated. He and different lab administrators are already bracing for the large ramp-up in testing they anticipate to start when the USDA order goes into impact Monday. However he does suppose extra must be achieved on the federal degree to encourage farmers to check their herds.
“At this level, farms simply aren’t volunteering samples as a result of they don’t have any incentives to boost their hand,” Poulsen stated. That data blackout makes it way more difficult for epidemiologists to hint the virus and perceive the way it’s spreading, the precise mechanisms of that are nonetheless unclear.
“We have to do what we will now to grasp it and comprise it so it doesn’t flip right into a pathogen of pandemic potential,” Poulsen stated. “That may be a actual danger if we proceed to disregard it.”