Based on cues she’d picked up from popular culture and public health guidance, Stanford Medicine statistician Maya Mathur, Ph.D., had always assumed that being overweight decreases lifespans. She was surprised, then, to come across research that suggested the life expectancy among overweight people—those with a body mass index between 25 and 29.9—wasn’t generally shorter than for people in the normal BMI range, controlling for factors such as age and whether they smoked.
In fact, a 2013 paper—which analyzed nearly 100 studies that included more than 2.8 million people—found that being overweight slightly reduced mortality risk. (That wasn’t the case for those considered obese, with a BMI at or above 30.) A 2016 analysis of around 240 studies did find a link between being overweight and higher mortality, but the effect was small.
Mathur felt that both studies had methodological problems, such as not controlling well for factors such as diet and physical activity.
“My own exposure to public health messaging suggested that an overweight BMI was a risk factor for mortality,” she said. But after reviewing the research she concluded, “That’s just not an evidence-based perception, considering the literature as a whole.”
Mathur, an assistant professor at Stanford Medicine’s Quantitative Sciences Unit and of pediatrics, wondered if doctors harbored the same misconceptions. Her mother, Vandana Mathur, is a practicing physician and biomedical researcher in the Bay area who’d learned in medical training that being overweight was harmful. With around one in three American adults qualifying as overweight but not obese, the pair decided to survey nearly 200 primary care physicians across the U.S. on how they viewed mortality risks for this group.
A gap between belief and reality
For their study, which was published in Epidemiology, the mother-daughter duo found that 90% of the surveyed doctors believed being overweight slashed patients’ lifespans, even though clinical guidelines from the American College of Cardiology and the American Heart Association say that being overweight is not linked to a higher risk of mortality.
“It seems there’s a really big gap between the empirical evidence and the physicians’ perceptions,” Mathur said.
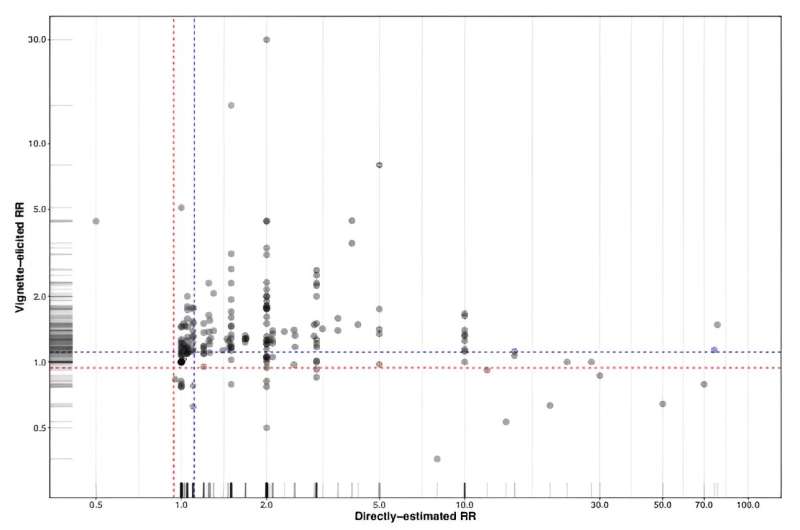
The researchers also gave doctors descriptions of two imaginary patients, 60-year-old women who were identical in every way, except one was overweight (but not obese) and one was normal weight. When they asked doctors to predict how likely each woman was to die from any cause in the next two decades, the physicians estimated that the overweight woman had a 25% higher mortality risk. When they asked physicians to estimate in general how being overweight affected mortality risk, the participants perceived a nearly 60% increase.
“The estimates they gave us were much stronger associations than even the studies that do suggest increased mortality risk,” Mathur said.
Mathur speculates that the mismatch could stem from misleading messages doctors get from the medical establishment. For example, the clinical guidelines that say being overweight doesn’t increase mortality risk also tell doctors to “advise overweight and obese adults that the greater the BMI, the greater the risk of…all-cause mortality.” The website of the Centers for Disease Control and Prevention similarly lumps together overweight and obese people, claiming that both are at increased risk of dying sooner from all causes.
“Perhaps the gap is really between the evidence and the communication,” Mathur said. Social stigma could also play a role. “It seems very plausible that our culture gives us a lot of messaging about BMI that’s not evidence based.”
Research does show that a higher BMI among overweight and obese people comes with a higher risk of coronary heart disease, cardiovascular disease, stroke and Type 2 diabetes, according to the American College of Cardiology and American Heart Association. But, Mathur says, “Much of the literature does not distinguish overweight from obesity.” Being obese or underweight are associated with elevated mortality risk.
Mathur says she’s concerned that doctors’ skewed views on weight could seep into interactions with patients. “Exaggerations about certain health risks could potentially cause undue stress for patients with an overweight BMI,” said Mathur. “And when the gap between communication and evidence comes to light, this could also, understandably, reduce patients’ trust in their doctors.”
Improving doctor-patient communication
Mathur urges doctors to stick closely to the research when talking to patients about weight. Such conversations are becoming more common as new weight-loss drugs, such as Ozempic, gain popularity. “It’s really critical to be respectful and non-stigmatizing, as well as evidence-based,” she said. “Focusing excessively on being overweight as its own risk factor for mortality, independent of biomarkers or metabolic health, does not seem warranted.”
Mathur believes future research could delve into the factors shaping physicians’ beliefs and how biases affect encounters with patients, as well as examining the views of doctors in other countries.
In the meantime, Mathur advises overweight patients who are bombarded with societal and public health messaging about weight to ask questions. “If it’s claimed that an overweight BMI is the key cause of a certain health issue or risk, ask, ‘What is the evidence for that?'” she said. “Perhaps there’s not as much you might think.”
More information:
Maya B. Mathur et al, Primary Care Physicians’ Perceptions of the Effects of Being Overweight on All-cause Mortality, Epidemiology (2023). DOI: 10.1097/EDE.0000000000001590
Citation:
What physicians get wrong about the risks of being overweight (2023, September 8)
retrieved 8 September 2023
from https://medicalxpress.com/news/2023-09-physicians-wrong-overweight.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.









