In my neurotech travels the commonest firms I encounter are these constructing digital dementia screening instruments. These are a category of mind well being assessments to see whether or not an individual might need, or be prone to creating, cognitive impairments that may very well be indicators of neurodegenerative illness.
The variety of folks with Alzheimer’s illness is on tempo to triple by 2060, as per CDC estimates. How finest to deal with them stays an open query, one which hinges on a extra fast query: Who’re we treating?
Bettering our capability to seek out folks dwelling with cognitive impairment entails figuring out what illness they’ve, earlier within the illness’s development. However doing this in an economical, patient-centered, physician-friendly method represents a key precedence for the likes of Bill Gates. And he’s not alone.
As I famous at this 12 months’s JP Morgan convention: “a neurotechnology dwelling run could be a dependable diagnostic take a look at (like a set of biomarkers) for earlier detection of delicate cognitive impairment and/or Alzheimer’s illness.”
Placing trial recruitment and digital endpoints apart for a second, let’s take into account the problem of discovering cognitive impairment in outpatient care. This drawback represents a possibility that would save hundreds of billions of dollars over the approaching a long time, whereas fundamentally changing the course of this illness and the seek for a remedy.
It’s a fancy and quickly altering market. Not all dementia is Alzheimer’s. Not all cognitive impairment is dementia. Not all screening is diagnostic. Funds are small, volumes are large. New instruments are coming, however outdated ones aren’t leaving; Subjective legacy assessments dominate pondering from medical faculty all through companies’ quarterly statements.
Early detection can change an individual’s life. But underreporting and stigma persist. Coaching and sources to undertake new instruments aren’t at all times out there.
For the healthcare system dealing with the “silver tsunami,” the necessity is obvious: Higher screening to seek out warning indicators, predict illness onset, and assist prioritize who will get a more in-depth examination.
Inside a Messy Market
Right now’s normal of care to judge cognitive well being includes an acronym salad of written or verbally administered cognitive assessments: MMSE, Mini-Cog, GPCOG, MoCA, SLUMS. These will be run by numerous medical employees and reimbursed by means of normal billing codes. Extra proprietary checks abound.
Most technology-based mind well being checks as we speak characteristic some interactive, proprietary screening course of. Sadly, on account of billing limitations, many “digital checks” are simply digital variations of the above assessments, although extra inventive instruments are rising.
Some startups emphasize quickness and affordability of use. Others emphasize objectivity by means of built-in biometrics. Just about all incorporate AI for scoring evaluation and normal reporting options for medical groups. No two instruments are the identical, however many are focusing on the identical drawback.
Past an getting older inhabitants and rising prevalence of illness, a number of enterprise pressures outline the rising market of dementia screening.
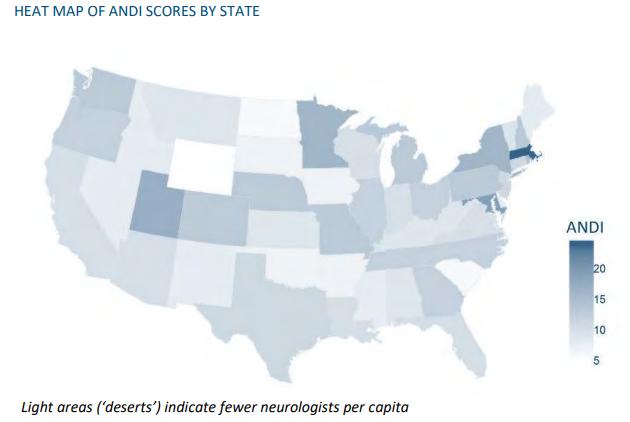
Alzheimer’s Illness and Associated Dementias Neurology Desert Index (ANDI), 2021
Neurology Deserts (2021)
- Physician Scarcity: Over 20 states are categorized as a “dementia neurology desert” by the Society of Actuaries. There are fewer than 10,000 practising neurologists within the US as per the BLS, or roughly 1 per 33,000 folks on common. HRSA predicts a 19% shortfall by subsequent 12 months. However that is about primary care, too: 85% of dementia sufferers are first recognized by non-specialists, however many main care physicians lack coaching and time to proactively assess cognitive well being of their sufferers. Rural areas have even higher shortages of each main and specialty care suppliers, underscoring the chance for scalable, easy-to-use checks.
- Regulatory Yahtzee: FDA has sanctioned quite a few units, apps, and algorithms to assist establish – however not diagnose – dementia. The company’s gatekeeping, whereas comprehensible, is sadly indifferent from medical observe. Their fragmented itemizing and lack of repairs or public steerage about these clearances and approvals signifies that bricky, “computerized” instruments cleared over a decade in the past might maintain extra market energy than as we speak’s leading edge tech. What’s extra: Poor coordination between federal businesses just like the NIA, NIH, CDC, and FDA on this single problem – dementia screening tools (p 59) – stands out as the nation’s greatest missed alternative to assist thousands and thousands of sufferers and households.
- Reimbursement: A $268 payment for cognitive evaluation go to, together with a handful of further CPT codes and modifiers tied to annual wellness visits, pre-and post-test analysis and interpretation, collectively create the medical marketplace for digital dementia screening. Nonetheless, CMS loves legacy assessments, just like the CDR scale or the FAST Screening, that are nonetheless thought-about dependable and standardized primarily as a result of they’ve been round for forty years. Have a look beneath and ask your self why solely an estimated 8% of older People dwelling with delicate cognitive impairment obtain a prognosis.
The FAST Scale is 40 years outdated. Time to improve?
High quality of Prognosis: Biology beats Digital
Given how outdated medical observe stays in terms of assessing dementia, biomedical science has fortunately introduced in higher levels of accuracy by means of pathological testing to establish organic presence of illness. Digital dementia screening matches into this broader panorama of diagnostics.
The gold normal for definitive prognosis of Alzheimer’s illness is the PET scan, which tags mind plaques with radioactive molecules (see this excellent history at Endpoints Information.) However these are time-intensive at two hours and up, costly, priced at $7-10k and better per take a look at, with solely about 2,500 PET scanners out there within the US.
Regardless of these less-than perfect circumstances, CMS removed reimbursement restrictions on PET scans final October, as a part of a market readiness push for brand spanking new remedies. After this modification, the variety of claims for PET scans quickly elevated by roughly 5x, as per Eisai’s latest briefing. However this isn’t a silver bullet: The pharma nonetheless missed their affected person enrollment goal by 80 percent.
Cerebrospinal Fluid (CSF) testing, involving lumbar puncture, additionally affords excessive accuracy, however carries appreciable expense, threat, and ache.
If there’s a silver bullet, it might be a blood take a look at.
“I feel there’s an excellent expectation that the blood take a look at may exchange the PET scan,” says Howard Fillit, cofounder and chief science officer on the Alzheimer’s Drug Discovery Basis (ADDF).
To this point, ADDF’s Diagnostics Accelerator has invested greater than $60 million in 58 initiatives, largely blood checks, and about one-fifth on digital approaches. Neurotech firms, take word: they’re currently open for proposals.
So whereas routine blood checks to detect Alzheimer’s illness appear to be imminent, within the US and globally, within the absence of those checks, and till their widespread rollout, frontline medical groups nonetheless require help.
Amount of Screening: Digital Beats Biology
Public Well being is a numbers sport: Once you’re speaking about 55 million folks world wide, blood checks versus digital checks is the mistaken debate. It comes all the way down to “diagnostic workflows” to triage threat and direct subsequent steps.
Digital dementia screening instruments are an early step in a course of that may additionally embody a routine bodily examination, aforementioned questionnaires, and “historian” (caregiver or member of the family) interviews, earlier than escalating to pathological checks to pin down a definitive prognosis (e.g. CSF, or quickly, blood checks).
These firms can not use the phrase “diagnostic,” reverting as a substitute to phrases like “evaluation” or “assistive” or “adjunctive.” In medical jargon, they’re medical choice help instruments that may be administered by medical assistants or ancillary employees with out in depth coaching.
However these instruments don’t exist in a void. AI-powered innovation is coming from all sides:
- Video games: Subsequent gen tools use clock-drawing, card-playing, shape-navigating, Augmented Actuality-questing, and numerous different interactive approaches to attain mind well being. Proof is rising that, at the least in comparison with yesterday’s questionnaires, these approaches are efficient.
- EHR information: In Medicare Benefit, and CMS’ GUIDE dementia care mannequin, startups are constructing care administration platforms that run on superior analytics, which researchers are validating can be utilized to foretell which sufferers develop Alzheimer’s illness.
- MRI scans: The FDA just approved the primary MRI-based, AI-enabled prognostic take a look at to foretell the way forward for “amnestic delicate cognitive impairment” and supply the chance of development to Alzheimer’s illness inside 5 years. AI-based MRI are altering medical look after stroke, most cancers, and mind harm; can they enhance dementia care, too?
- EEG: Firms like Cognision and VoxNeuro are bringing EEG-based assessments of cognitive operate into the medical setting. If biomarker-based approaches cross over from analysis curiosity to practice-based instrument, alternatives to combine medical trial recruitment into medical observe extra tightly may very well be a win-win for public well being and life sciences.
On the horizon, eye testing, vocal biomarkers, and different neurotechnologies are in analysis and growth. However even when the science and know-how behind all of those improvements are legitimate, it received’t matter a lot till they attain the outpatient market as a usable and cost-effective a part of medical observe.
RIDDLE Me This: A Lengthy-Time period Answer?
How can a time and cash-strapped neurology or main care observe resolve what screening instruments are finest, or in what order to make use of them? EHR analytics earlier than wellness visits? Video games within the ready room? MRI earlier than care plan? Or, simply wait till blood checks develop into out there?
The Alzheimer’s Affiliation, maybe essentially the most influential physique for practising physicians, is engaged on solutions. Dr. Rebecca Edelmayer, senior director of scientific engagement, recently said, “The sphere is shifting so quick…Even the suggestions we put out this 12 months—seemingly they’ll should be up to date once more inside a 12 months.”
What’s extra: Past with the ability to stratify and reliably diagnose sufferers, the economics of what occurs subsequent are one other quagmire. The handoff between outpatient clinicians and medical trials recruitment requires further affirmation testing, which varies by every mixture of medical analysis group, pharma sponsor, and insurer.
What about Pharma’s newly authorized and soon-coming IV-based medicine focusing on amyloids? Altering prescriber habits stays a thorny path, involving heavy but unknown administrative lifts and overhead bills to coordinate visits, imaging, reporting, in addition to rigorous medical monitoring and compliance.
Once more: Eisai, with an $11B market cap and the only real drug available on the market, couldn’t meet the wants of 80 % of the folks looking forward to therapy. We’re not there but.
One neurotech chief government I requested about these enrollment woes was blunt: “There’s simply not a adequate incentive for physicians to diagnose these sufferers. It’s not nearly getting paid transactionally – in the event you’re a doctor working a observe, you’re nervous about what’s subsequent: extra questions, extra legal responsibility, extra compliance. It’s a straight up damaging incentive construction.”
His short-term concept was “lining up critical fee to get docs to do that.”
For a longer-term strategy, I’d eschew the US federal authorities’s byzantine National Plan – whereby a multimillion greenback digital screening toolkit constructed by a analysis arm shouldn’t be endorsed for official medical use by both the regulatory or the fee arm – and switch as a substitute to Europe.
The Real-World Implementation, Deployment, and Validation of Early Detection Tools and Lifestyle Enhancement (AD-RIDDLE) is a 24-member collaborative testing out the actual world economics of an Alzheimer’s Illness toolbox, utilizing a shortlist of government-cleared (CE mark) instruments in sync with lab checks, medical workflows, longitudinal monitoring, and real-time proof era.
Whether or not or not it really works, the coordinated strategy is the notable innovation.
Validation, Deployment, and Actual-World Implementation of a Modular Toolbox for Alzheimer’s Illness … [+]
AD-RIDDLE “envisions the continuum of AD screening, prognosis, and therapy as a pipeline, and proper now, that pipeline is advanced. The venture goals to take aside the pipes, establish the obstacles and their location, and put them again collectively once more in order that affected person and supplier can circulation extra easily, making a troublesome course of extra environment friendly, efficient, and patient-focused.”
Innovating On Shifting Sands
So, what does this all imply for neurotech startups, traders, and companions angling for alternatives to enhance dementia screening?
Brief-term, R&R (regulation & reimbursement) is hard, however don’t overlook the worth of denting the variety of undiagnosed sufferers and getting a foothold within the medical market.
Mid-term, diversify income. Life sciences is an apparent market, with much less regulation in alternate for what one CEO referred to as “lumpy” (learn: sporadic) contracts. Life insurers, analysis teams, and overseas markets are all shopping for. Direct pay clinics, different neurotech firms, and even shoppers would possibly develop into markets, too
Lengthy-term, don’t underestimate the worth of participating straight with affected person and caregiver communities as you map the following era of your product. Their skilled information of dwelling with dementia hardly components into the above challenges, making them the biggest underserved market on the earth – one with untold untapped alternatives to enhance effectivity and affect of medical care, drug trials, and even federal coverage.